During Suicide Prevention Week, People of Color’s Mental Health Struggles Cannot be Forgotten
National Suicide Prevention Week runs from Sept. 8–14 to raise awareness about suicide and the resources available to help those struggling with mental health crises. However, certain demographics seem to consistently slip through the cracks of mental health education, advocacy and care. People of color in the United States suffer from mental illness at rates similar to those of white people, but often do not receive adequate care.
According to the American Psychiatric Association, ethnic and racial minorities often bear a disproportionately high burden of disability caused by mental disorders. Though rates of diagnosed depression are lower in Black (24.6%) and Hispanic (19.6%) populations than in whites (34.7%), depression in Black and Hispanic communities is likely to be more persistent and severe. African American adults are 20% more likely to report serious psychological distress than white adults. American Indians/Alaska Natives report higher rates of posttraumatic stress disorder and alcoholism than other racial and ethnic groups.
Native American youth have the highest suicide rate out of any racial group.
In 2015, among those with mental illnesses, nearly half of white people received services. However, only 31% of both Blacks and Hispanics and 22% of Asians received care.
Reasons for non-white people not getting the treatment they need include systemic barriers, such as lack of insurance, mental illness stigma often more common in minority populations, language barriers, distrust in the healthcare system and lack of diversity and cultural competence in mental healthcare providers, according to the American Psychiatric Association.
Additionally, the compounding stresses of racism, xenophobia and the social, economic and emotional problems they cause are a burden white Americans simply do not have to face.
According to the Center for Medicare and Medicaid Services Office of Minority Health, (CMS) those identified as multi-ethnic were the most likely minority group to report poor mental health and to be unable to participate in daily activities due to mental health problems.
The CDC recommends employers address mental health in the workplace and provide benefits that cover mental health care.
The adoption of mental health-related employee resource groups (ERGs) is also growing. Mindsharepartners.org created a comprehensive list of companies that offer ERGs that address mental wellness.
Johnson & Johnson, a DiversityInc Hall of Famer that appears no. 7 on DiversityInc’s 2019 specialty list, “Best Companies for Employee Resource Groups,” has an ERG called Mental Health Diplomats. Accenture (no. 7 on 2019 Top Companies for Diversity), EY (no. 6 on “Best Companies for People with Disabilities” and no. 1 on “Best Companies for Employee Resource Groups”) and Kaiser Permanente (no. 14 on “Best Companies for People with Disabilities”) all have ERGs that discuss mental illness.
The National Alliance on Mental Illness cites homelessness and exposure to violence as factors that greatly affect African Americans’ mental health. Black people make up about 13% of the U.S. population, but 40% of the U.S. homeless population. Additionally, the National Alliance on Mental Illness states African American children are more likely to be exposed to violence than other children.
Many people of color, especially Blacks, report distrusting the healthcare system, and with good reason. This fear and distrust stems from a long history of doctors mistreating, abusing and testing on Black bodies without their consent, dating back to slavery. Eugenicist government programs in the 20th century led to the coerced sterilization of thousands of men and women throughout the U.S. These government-funded programs were used to “control” “undesirable” populations, including immigrants, people of color, poor people, single mothers, the disabled and the mentally ill.
Today, mental health care still fails people of color. A study published by PubMed Central (PMC) found that after entering care, minority patients are less likely than white patients to receive the best available treatments for depression and anxiety.
The effects of mental illness in communities of color contribute to the cycle of oppression. Children of color with behavioral issues are more likely to end up in the juvenile justice system due to harsher punishments they face in schools, according to the American Psychiatric Association.
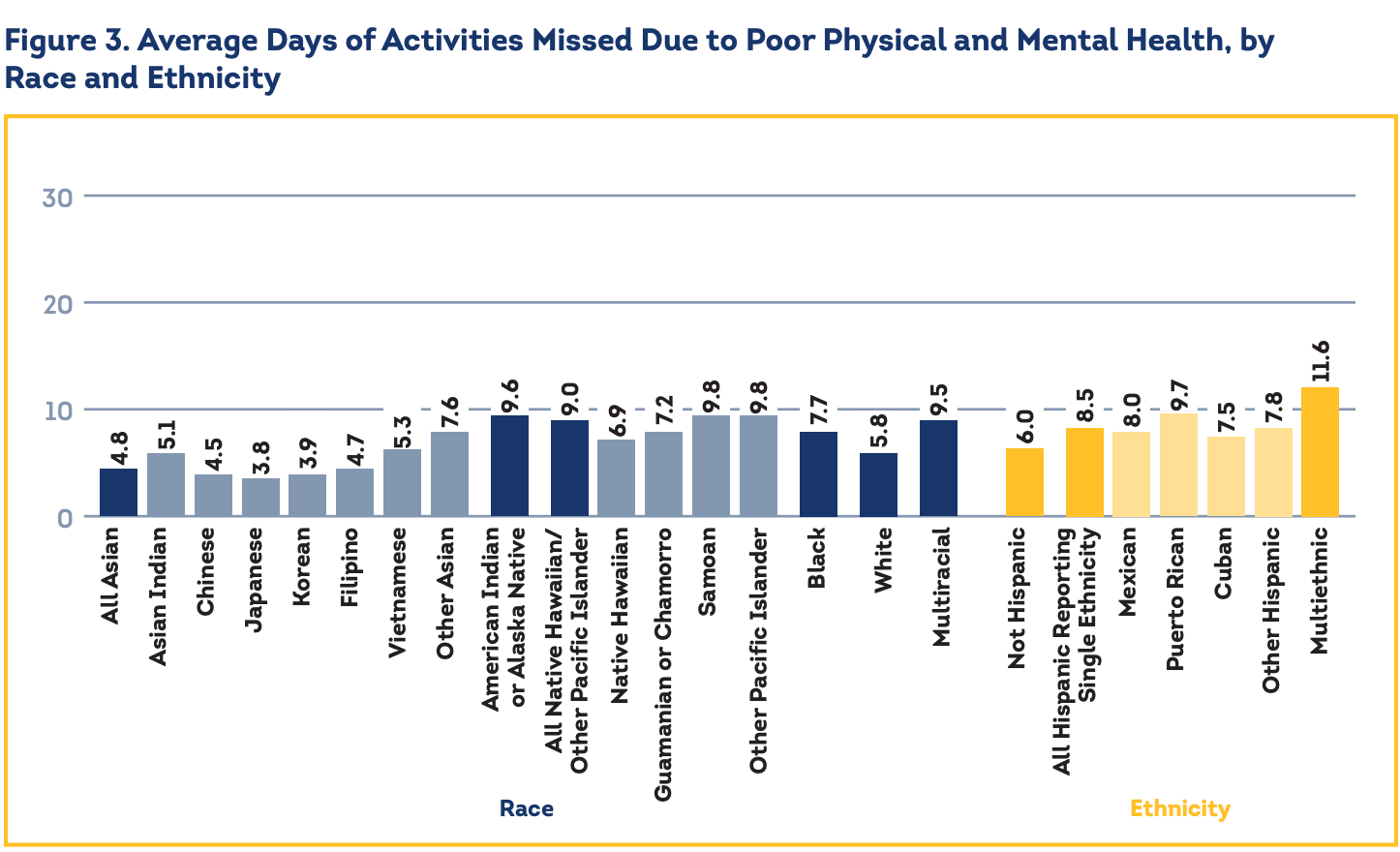
Mental and behavioral disorders are among the leading causes of disability in the U.S. because they affect people’s abilities to work and perform other daily activities. CMS shared data on people of different races and ethnicities who reported the average number of days of activities they missed as a result of mental illness.
White respondents reported an average of 5.8 days, Black respondents reported an average of 7.7 days, American Indian and Alaska Native respondents reported an average of 9.6 days and all native Hawaiian and other Pacific Islander respondents reported an average of 9.0 days.
Hispanics reporting a single ethnicity reported 8.5 days, and multiethnic people reported 11.6.